🧩 What’s Happening
When families challenge the denial of Intermediate Care Facility (ICF/IID) care or any other Massachusetts Department of Developmental Services (DDS) decision, the hearing process is controlled, undermining due process.
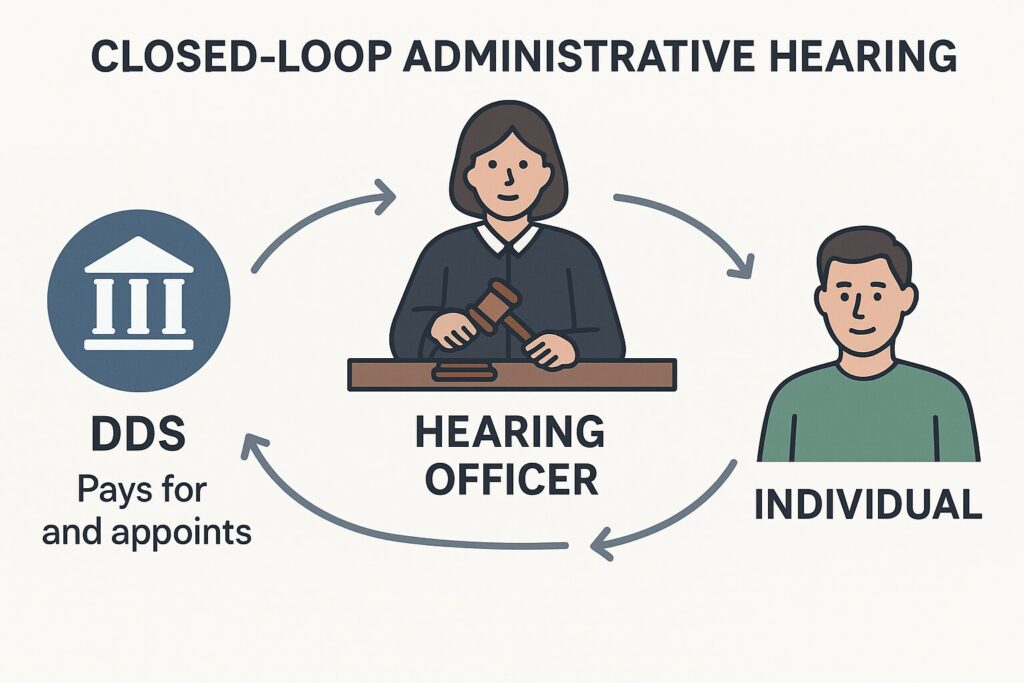
As a result, administrative DDS hearings are a closed loop of self-validation, where the agency that made the decision also controls the appeal and the outcome.
Consider that the hearings are:
- Controlled by the Massachusetts Department of Developmental Services (DDS), the same agency that denied the service
- Staffed by hearing officers appointed and paid by DDS
- Based on evaluations conducted by DDS-contracted providers
- Dismissive of requests for independent evaluations
🚨 Why This Violates Federal Law
1. Due Process Requirements
Federal Medicaid law requires that appeals be:
- Impartial
- Accessible
- Based on evidence, not agency loyalty
The hearing must be conducted by an impartial official who was not involved in the original decision.
— 42 CFR § 431.240(a)
Given these facts, Massachusetts DDS may be violating due process requirements when:
- The hearing officer is financially or professionally tied to DDS
- The officer refuses to consider independent evaluations
- The process rubber-stamps agency decisions without scrutiny
2. Right to Independent Medical Assessment
Families have the right to challenge service denials with credible, independent clinical evidence.
The individual must be allowed to present witnesses and evidence.
— 42 CFR § 431.242
Refusing to order or consider independent evaluations violates this right.
🧠 Why This Matters
When the same agency controls the evaluation, the denial, and the appeal:
- Families are denied a fair chance to prove medical necessity
- Individuals with profound disabilities are blocked from accessing ICF/IID care
- The system protects providers—not people
This is not just unethical. It may be unconstitutional under the principles of procedural due process.
To understand better about the ramifications of biased hearings, click here.
