Introduction to Our Five Part Series: MA Intellectual and Developmental Disabilities (IDD) Federal Lawsuits
Massachusetts is often praised as a national leader in disability services. The state repeats this claim in legislative hearings, agency reports, and public messaging. But the historical record tells a very different story, one in which progress has come not from vision or leadership, but from federal judges, class‑action lawsuits, and decades of court‑ordered reform
For more than fifty years, families have turned to the courts because every other avenue failed them. And each time, the courts uncovered the same underlying truth: Massachusetts does not protect the rights of people with intellectual disabilities unless it is forced to.
This series examines four major lawsuits — Rolland, Ricci, Boulet, and Hutchinson. These cases reshaped the state’s disability system.
What Is An ICF?
An ICF/IID (Intermediate Care Facility for Individuals with Intellectual Disabilities) is a federally regulated residential program for people with intellectual and developmental disabilities that provides 24‑hour nursing, clinical oversight, and active treatment — a level of care that community group homes are not required to offer. Learn more about ICF/IID care here.
Each case involved a different population, a different setting, and a different set of failures. Yet together, they reveal a single, unmistakable pattern:
- The state ignores systemic problems until families sue.
- The courts intervene.
- The state complies only under pressure.
- And once oversight ends, the system drifts back into crisis.
These lawsuits are not ancient history. Their themes echo in today’s collapsing day habilitation programs, unsupported group homes, rejected high‑acuity individuals, and the quiet return of custodial institutionalization in community-based services and nursing homes.
This pattern does not only affect adults. The Pappas Rehabilitation Hospital for Children historically included an ICF‑level program for children with profound disabilities. Years ago, the state eliminated that ICF‑level program, and medically fragile children who needed that level of care were placed in “pediatric nursing homes” because no pediatric ICF existed anywhere in Massachusetts. Later, under pressure from Rolland’s restrictions on nursing home placements, the state attempted to move these children into group homes despite their complex medical needs. Families protested and won an agreement allowing their children to remain in the pediatric nursing home with added active treatment — essentially creating an ICF‑level program inside a nursing facility.
Today, the state is dismantling Pappas again. The administration announced plans to close the hospital, then walked back the announcement after public pushback, yet students are being discharged one by one. The state now proposes creating a small pediatric unit at Western Massachusetts Hospital in Westfield, but this does not replicate the specialized, long‑term, habilitative environment that Pappas provides. The dismantling of Pappas is not an isolated event. It is the latest expression of the same systemic failures that have driven families to court for decades.
Across five decades, the state has repeatedly chosen the cheapest, least disruptive administrative option — even when it meant uprooting people, dismantling programs, or placing individuals in settings that stripped away their rights.
This series is not about nostalgia, blame, or policy theory. It is about truth.
And the truth is this: Massachusetts has been sued again and again because it has never built a system capable of meeting the needs of the people it claims to serve.
Only by understanding this history can we understand the crisis unfolding today.
Why We Begin with Rolland v. Cellucci
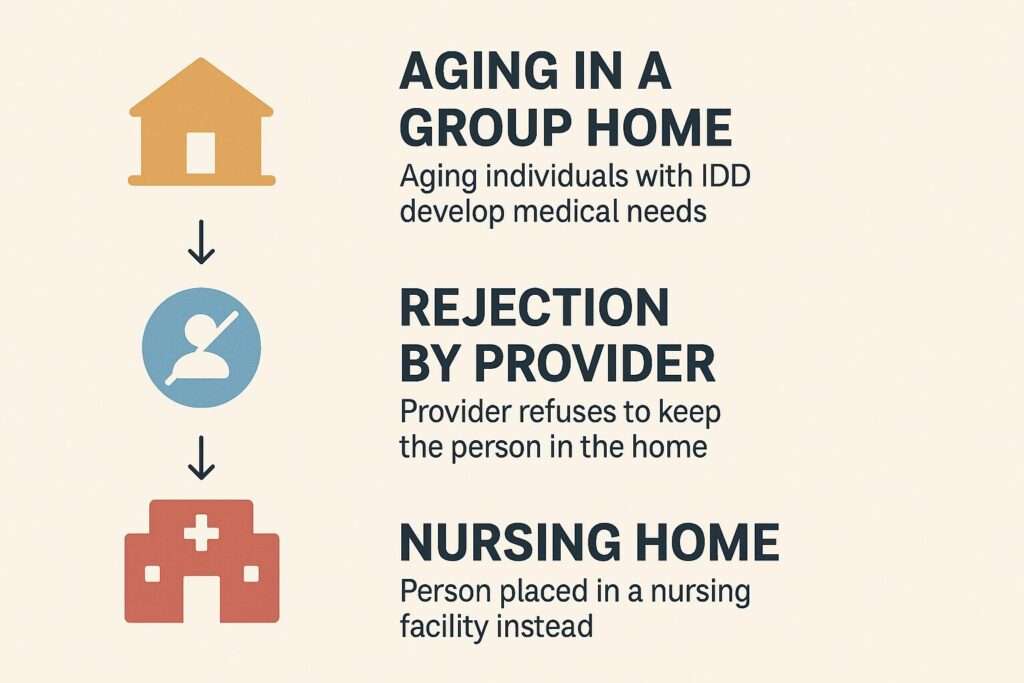
Most families believe that once their adult loved one is settled in a group home or shared living arrangement, they will be set for life. They imagine aging in place, surrounded by familiar staff, routines, and peers. They assume that the provider who has cared for their son or daughter for decades would never simply say, “We can’t handle them anymore.”
But Rolland showed us the truth.
In the wake of the Ricci lawsuit — a case that pushed Massachusetts to expand community placements — the state sought to show quick progress. Rather than creating high‑acuity community homes or maintaining appropriate ICF placements, it quietly moved medically complex residents from ICF/IID facilities into nursing homes, where there was no habilitation, no integration, and no meaningful life. These were not temporary placements. They were long‑term warehousing solutions that allowed the state to claim progress while abandoning the very people it no longer wanted to serve. The Massachusetts Department of Developmental Services (DDS) allowed it. Families were powerless to stop it. And without access to high‑acuity care, nursing homes became the default, not because they were appropriate, but because they were available. Our cost analysis shows that this default was not accidental. DDS consistently relies on services that fall outside its own budget—such as MassHealth‑funded nursing homes, day habilitation, and hospital emergency services. This creates a perverse financial incentive to shift aging individuals out of the DDS system entirely, which is precisely the dynamic that led to the Rolland lawsuit.
Families didn’t choose this.
They didn’t agree to it.
They didn’t even know it was possible.
And by the time it happened, many parents and guardians were already gone — leaving no one to fight the decision on their behalf.
Rolland exposed a system that quietly moved people into nursing homes because it was cheaper, easier, and politically invisible.
And unless we act together, it will happen again.
Rolland v. Cellucci — When Massachusetts Sent People with Intellectual and Developmental Disabilities to Nursing Homes
The first lawsuit in our series is also the most chilling. Rolland v. Cellucci revealed that Massachusetts moved medically complex residents out of ICF/IID facilities and into nursing homes even after Ricci had strengthened ICF/IID care. These ICFs were fully capable of supporting individuals with significant medical needs. Creating comparable high‑acuity community homes would have required staffing and resources the state was unwilling to invest. Rather than maintain or expand appropriate ICF/IID care, Massachusetts took the easiest path and shifted residents into nursing homes — settings with medical care but no active treatment, no habilitation, and no meaningful life.. These were not isolated cases. They were systemic, sanctioned, and ongoing.
Rolland showed, with devastating clarity, how easily the state could uproot people from stable homes and place them in settings that stripped away their rights and their lives.
This pattern continues today. The administration’s current ‘consolidation’ initiative — breaking up long‑standing group homes and moving residents into any available bed to save money — shows that individuals in Home and Community Based (HCBS) group homes do not have true tenancy or stability. These are not their own homes; they are placements controlled by private corporate providers and the state.
If you think your loved one is safe in their group home forever, Rolland will make you think again.
→ Read Part 1: Rolland v. Cellucci coming next week.
→Read Additional Context below to find out why the Western Massachusetts Hospital in Westfield (aka, Westfield Hospital) is not an adequate replacement for the Pappas Rehabilitation Hospital.
Additional Context: Why Western Massachusetts Hospital Is Not an Adequate Replacement for Pappas
Western Massachusetts Hospital in Westfield (WMH) is an adult chronic‑care hospital, not a pediatric ICF‑level program.
The state’s proposal to create a small pediatric unit at WMH does not replicate the clinical, educational, or habilitative environment that Pappas provides. WMH is designed for adults with long‑term medical conditions, not children with complex developmental disabilities who require integrated schooling, therapies, and habilitation.
The proposed unit is dramatically smaller and cannot meet statewide need.
Pappas has historically served far more children than the 25‑bed unit proposed for WMH. A downsized program means fewer placements, longer waits, and more children pushed into inappropriate settings.
WMH lacks the on‑site educational and therapeutic infrastructure that defines Pappas.
Pappas integrates medical care with a full school program, adaptive recreation, behavioral supports, and habilitation. WMH does not have a pediatric school, pediatric therapists, or the developmental programming required under federal law for children with significant disabilities.
The move isolates families and disrupts continuity of care.
Pappas serves families across the state. Relocating children to a single adult hospital in Western Massachusetts creates geographic barriers, reduces family involvement, and undermines the stability that medically fragile children depend on.
The transition is happening without a true replacement in place.
Despite public assurances that Pappas is “not closing,” students are being discharged one by one before the WMH unit is operational. This mirrors past patterns in which the state dismantles specialized programs first and improvises alternatives later — often at the expense of children’s safety and development.
The plan repeats a familiar pattern: eliminate ICF‑level care without creating an equivalent alternative.
Just as adults lost access to ICF/IID placements, children are now losing access to pediatric ICF‑level care. The WMH proposal is not a replacement; it is a reduction.
