⚖️ Legal Analysis: Evaluations and Denial of Intermediate Care Facility (ICF/IID) Care
Overview of Massachusetts Practices
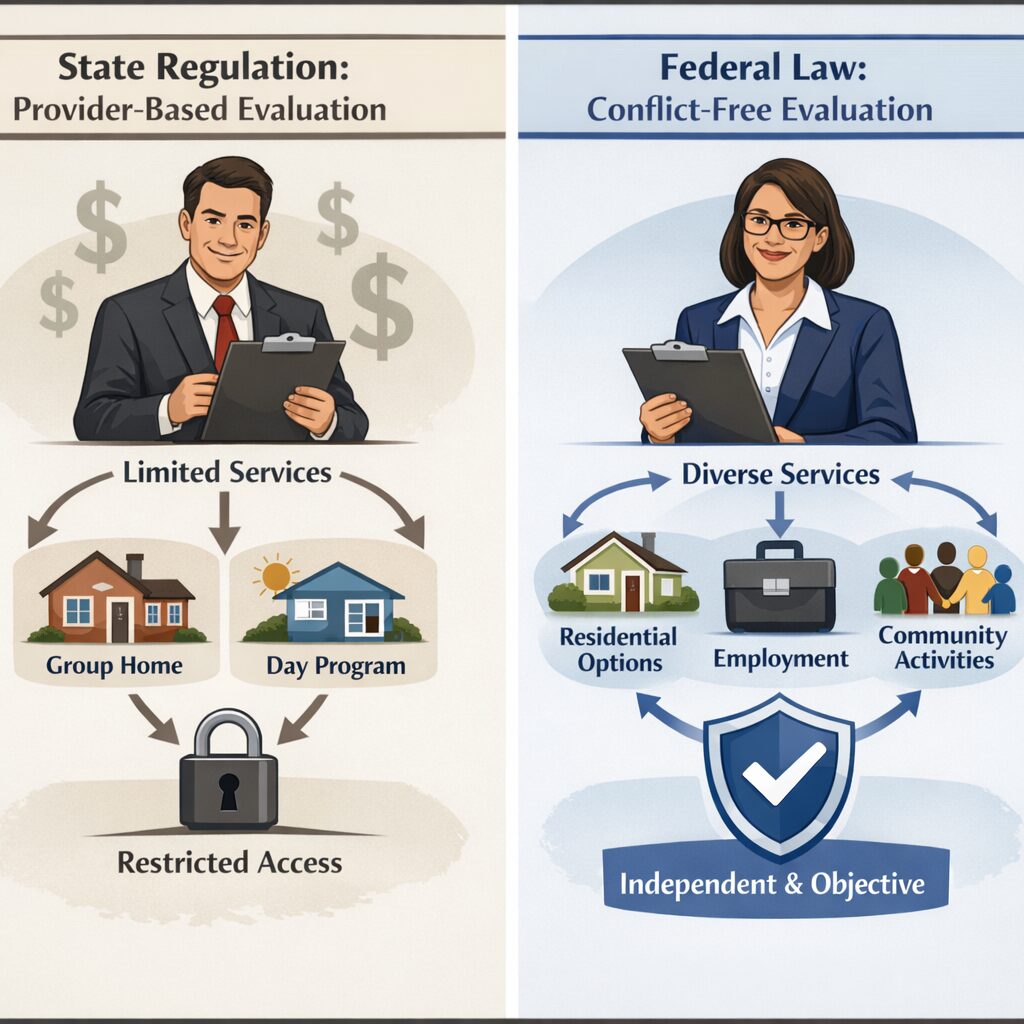
The Massachusetts Department of Developmental Services (DDS) requires corporate providers, who possess financial and operational interests in community-based services, to conduct support evaluations for individuals with intellectual and developmental disabilities (IDD). These evaluations frequently:
- Recommend only those services that the provider currently offers
- Overlook or omit critical aspects of an individual’s medical, behavioral, or safety needs
- Restrict access to ICF/IID admission pathways for families
Such practices present a clear conflict of interest, impacting the integrity and fairness of assessments required for proper care.
Federal Law Requirements
Medicaid Entitlement
- Under federal Medicaid law, states are obligated to provide ICF/IID services to individuals meeting the required level-of-care criteria.
- All evaluations must be objective, person-centered, and clinically appropriate.
- Denials based on provider preference contravene individuals’ legal entitlement.
States must ensure that services are sufficient in amount, duration, and scope to reasonably achieve their purpose.
— 42 CFR § 440.230
Freedom of Choice
Individuals retain the right to select among all available Medicaid services, including institutional care.
A recipient may obtain services from any qualified provider
— 42 CFR § 431.51
Due Process and Fair Hearings
Families must be informed of their rights to appeal service denials and request independent evaluations.
The agency must provide an opportunity for a fair hearing to any individual whose claim for services is denied.
— 42 CFR § 431.220
Possible Unlawful Practices
The current DDS approach may violate:
- Federal Medicaid regulations governing service access and freedom of choice
- Due process protections under the Social Security Act
- The principles established by Olmstead v. L.C., if institutional care is denied without proper evaluation
Additionally, this policy contradicts CMS guidance that mandates ICF/IID services be available to those whose medical needs justify such care—not only to those who cannot be maintained in community placements.
Analysis of Massachusetts Regulation 115 CMR 6.22(4)(b) in Light of Federal Law
Regulation Summary:
Under 115 CMR 6.22(4)(b), assessments and consultations relating to service planning must be performed by the individual’s current provider, even when that provider has vested financial or operational interests in the outcomes.
This arrangement results in:
- Service decisions made solely by the existing provider
- Routine exclusion of ICF/IID care regardless of necessity
- Lack of independent, objective assessment options for families
Federal Law Violations
Conflict of Interest Compromises Medical Necessity
- Federal Medicaid law stipulates that services must be determined by clinical need alone.
- When providers evaluate their own clients, recommendations are typically limited to existing service offerings, often excluding necessary ICF/IID care.
Denial of Freedom of Choice
- Medicaid recipients are entitled to choose among qualified providers and service types.
- Current state regulations restrict this choice by requiring evaluations through one self-interested party.
Compromised Due Process
- Independent evidence and challenges to evaluations must be permitted.
- Mandating provider-based assessments eliminates opportunities for unbiased clinical input.
Real-World Implications
- Individuals with significant disabilities may not access needed ICF/IID care.
- Families encounter systemic barriers due to overlapping evaluator, planner, and provider roles.
- Appeals are less effective when hearing officers rely on potentially biased assessments.
Government Accountability Office’s (GAO) Person-Centered Planning Requirements
The GAO has advised the Centers for Medicare and Medicaid Services (CMS) to require person-centered planning free from conflicts of interest; however, Massachusetts regulations enforce such conflicts. Federal Medicaid regulations unambiguously prohibit conflicts of interest in needs assessments (see: 42 CFR 441.301(c)(1)(vi), 42 CFR 431.10), yet state rules mandate otherwise (see: 115CMR6.22(4)(b)).
A retired judge reviewed our legal analyses for clarity and accuracy. Our website is intended for educational and advocacy purposes only and does not constitute legal advice
