Defending Access to Intermediate Care Facilities for Individuals with Intellectual Disabilities (ICF/IID) Care for People with Severe Disabilities
🔍 Are Individuals with Intellectual Disabilities Entitled to ICF/IID Care?
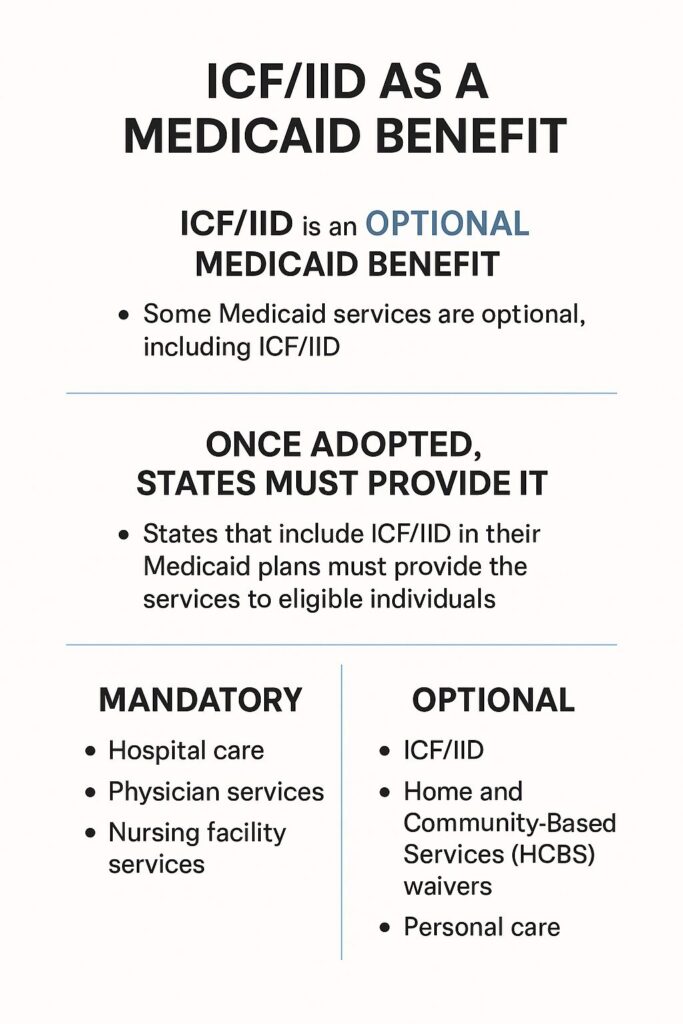
Medicaid is a federal-state program that guarantees coverage for medically necessary services to eligible individuals. While some services are federally mandated, others — like Intermediate Care Facilities for Individuals with Intellectual Disabilities (ICF/IID) — are optional benefits.
However, once a state includes ICF/IID in its Medicaid plan, it is legally obligated to provide those services to eligible individuals.
• ICF/IID is optional at the federal level:
States are not required to include it in their Medicaid plans.
• But once adopted,
it becomes a legal entitlement within that state:
Eligible individuals must be served under the terms of the state’s Medicaid plan.
• Mandatory services include things like hospital care, physician services, and nursing facility services. These must be provided in every state.
• Optional services include ICF/IID, Home and Community-Based Services (HCBS) waivers, personal care, and others. States choose whether to include them.
🏥 ICF/IID Services Are Federally Defined
Intermediate Care Facilities for Individuals with Intellectual Disabilities (ICF/IID) are federally defined under the Social Security Act and regulated by the Centers for Medicare and Medicaid Services (CMS).
States must:
- Offer ICF/IID services to individuals who meet level-of-care criteria
- Maintain sufficient capacity to meet demand
- Ensure timely access without unnecessary barriers
Key Point:
Massachusetts cannot lawfully restrict ICF/IID access by policy, budget, or ideology.
⚖️ Legal Foundations
- Social Security Act, Title XIX (Medicaid): Defines ICF/IID as a mandatory benefit once a state chooses to include this in their state Medicaid plan.
- CMS State Operations Manual Appendix J: Details standards for ICF/IID care and resident rights
🚫 What Violates Medicaid Entitlement and Disability Rights Protections?
- Denying access to ICF/IID services for eligible individuals when the state includes ICF/IID in its Medicaid plan
→ Once a state elects to offer ICF/IID, it must provide it to those who meet clinical and programmatic criteria. - Requiring individuals to “fail” in community placements before considering ICF/IID
→ This may violate the ADA and Olmstead v. L.C. by coercing placement in less appropriate settings and delaying medically necessary care. - Closing facilities without ensuring access to equivalent care for displaced residents
→ States must ensure continuity of care and uphold Medicaid’s guarantee of access to covered services. - Delaying or denying admission based on non-clinical factors (e.g., cost, ideology, administrative preference)
→ Medicaid decisions must be based on medical necessity and eligibility, not subjective or financial bias. - Failing to assess individuals for ICF/IID eligibility when clinically indicated
→ States must conduct person-centered evaluations and offer all covered services for which an individual qualifies
🧠 Why This Matters
These practices can violate:
- Medicaid’s entitlement structure under Title XIX of the Social Security Act
- Federal regulations including 42 CFR § 440.150 and § 483.440
- Civil rights protections under the ADA and Olmstead decision
They may also trigger:
- Due process violations
- Federal oversight or corrective action
- Legal challenges by families and advocates
Legal Resources:
- CMS Medicaid Services Overview
- 42 CFR § 440.150 – ICF/IID Services
- CMS State Operations Manual – Appendix J
For more information on how states like Massachusetts still deny access to ICF/IID care, click the button below:
